
5 great tips for sustainable summer living

Sustainable living treads lightly on natural resources and follows a rethink, reuse, repurpose mantra to minimize waste.
Big and small wallet-friendly tips can help you save money and befriend our planet this summer, says Dr. Wynne Armand, a primary care physician at Harvard-affiliated Massachusetts General Hospital, and associate director of the Mass General Center for the Environment and Health. Here are five great tips to get you started.
1. Embrace the 5 Rs
Refuse, reduce, reuse, repurpose, and only then recycle is a well-laid out sustainability strategy promoted online by the Cincinnati Recycling and Reuse Hub. Do you really want or need a shiny new object? Where can you share tasks or tools? What could you swap, give away, or buy used? How could you slim down your recycling stream?
Give yourself permission to start here: Nobody is perfect. We all have preferences and sustainability blind spots, fumbles, and “sorry, just no” feelings. Start where you are and add on when you can.
2. Cut down on cooling energy
Summer heat can endanger your health, and paring back on energy use isn’t always possible or wise. Still, it may be possible to:
- Stay cooler naturally. Pull down shades during daytime hours to block out hot sun. Open windows at night if the temperature cools down, and to capture cross breezes if possible. Dress in loose cotton clothes and wear a shading hat when outdoors. Remember that sun bounces off lighter colors and is soaked up by black or darker colors. Make your own shade by carrying an umbrella on sunny — not just rainy — days. “Prepare meals that don’t require cooking or baking, since that saves resources and keeps your home cooler,” advises Dr. Armand.
- Seek shade and cool spots. If you don’t have air conditioning or you worry about the bills, green, leafy spaces like parks can help cool you down. Cities and towns often open cooling centers, splash pads, and public pools. Public buildings like libraries and malls are available during daytime hours for anyone trying to beat the heat.
- Turn up the temperature. On air conditioning, that is. If you’re fortunate enough to have air conditioning at home, follow natural cues. When you’re shivering, sweater-seeking, or tucked up under blankets, push the temperature up to save energy and money.
3. Save resources
A sharp eye for energy savings may help pare down bills, too.
- Electrify. Shrink your carbon footprint and help cut air pollution by using electric grills, mowers, and other landscaping tools. When tools or appliances need to be replaced, consider electric options.
- Conserve energy. Turn off electrical equipment that is not in use in the office and at home, such as lights, TVs, computers, copiers, and printers.
- Go low when demand is high. “During peak electricity demand, ensuring stability of the grid is essential to public health,” says Dr. Armand. “Avoid using appliances like dishwashers, washers, or dryers during periods of high demand. Instead, do these chores — and charge your electric car, if you have one — late at night.” Some energy-hogging appliances have timers to help with this.
- Sign up for Shave the Peak alerts. Know when to curb your electricity use to avoid times when your local electric grid is relying on nonrenewable, expensive, polluting fossil fuels.
4. Stay heat-aware and hydrated
Saving resources is a worthy goal, but not at the expense of staying safe and healthy when summer temperatures spike.
- Make plans to stay cool. When summer swelters, having an affordable, personal plan to cool down — especially during heat waves — can be lifesaving.
- Watch out for signs of dehydration. Drinking plenty of water and eating water-rich foods like lettuce, cucumbers, melon, and citrus fruits can help you stay well hydrated. Water-filling stations for reusable bottles cut down on single-use plastic bottles and help save money at the grocery store.
- Know how to treat heat rash and more serious heat-related illnesses. The small, itchy red or darkened bumps of heat rash (prickly heat) occur when sweat ducts become blocked or inflamed. This makes it harder for children and adults to cool their bodies down. Generally, too much heat can harm our bodies, particularly if we work outdoors, take certain medicines, or have certain illnesses.
5. Kickstart sharing circles
Sharing circles can help you expand a wardrobe, tool shed, or taste in foods — all while building community.
- Start local, then consider expanding. Brainstorm with a few friends on what you all might like to share or swap. Think seasonal: gardening tools, outside décor, summer sports (because not everyone needs to own a paddleboard). Local clubs, block associations, or public spaces like libraries and schools may be willing to host community swaps and shares. Some communities have swap sheds and some libraries loan gadgets and even appliances like a portable induction cooktop burner, tech and home-improvement tools, games, and much more.
- Summer supper club. Perfect for those overloaded with summer harvests from window boxes, community gardens, or a CSA share. Build a theme around what’s fresh, local, and low-cost. Plant-forward menus are good for health and for the planet. Cultural inspiration always helps. And having one person cook — or stressing no-cook recipes — saves resources.
- Cut your clothing allowance. Tired of your wardrobe? Gather friends for a summer clothes and accessories swap. Be sure to agree on rules: gently-used, carefully washed, no stains, and so on.
- Hot spots. “Gathering at a friend’s or neighbor’s home for fun games and festivities on hot days is a great way to build community while saving on energy costs for cooling. And rotate for that next hot day!” says Dr. Armand.
About the Author

Francesca Coltrera, Editor, Harvard Health Blog
Francesca Coltrera is editor of the Harvard Health Blog, and associate editor of multimedia content for Harvard Health Publishing. She is an award-winning medical writer and co-author of Living Through Breast Cancer and The Breast Cancer … See Full Bio View all posts by Francesca Coltrera
About the Reviewer
Howard E. LeWine, MD, Chief Medical Editor, Harvard Health Publishing
Dr. Howard LeWine is a practicing internist at Brigham and Women’s Hospital in Boston, Chief Medical Editor at Harvard Health Publishing, and editor in chief of Harvard Men’s Health Watch. See Full Bio View all posts by Howard E. LeWine, MD

Ultra-processed foods? Just say no

Americans love their ultra-processed foods, whether they come as cereal (like Cap’n Crunch, a favorite of mine as a kid), snack foods (like Cheetos), entr’es (like hot dogs), or desserts (like Twinkies). Sure, loading your plate with vegetables, fruits, fish, healthful oils, and grains in a Mediterranean-style diet boosts heart and brain health. But if you also eat some ultra-processed foods, is that bad for your brain health?
What to know about this new study
A new study appears to deliver resounding yes: eating ultra-processed foods is linked to a greater risk of cognitive impairment and strokes.
This well-designed observational study examined data from the REGARDS (REasons for Geographic And Racial Differences in Stroke) project, a longitudinal study of non-Hispanic Black and white Americans ages 45 years and older. Study participants were initially enrolled between 2003 and 2007 and were given a number of questionnaires evaluating health, diet, exercise, body mass index, education, income, alcohol use, mood, and other factors. In addition, tests of memory and language were administered at regular intervals.
To examine the risk of stroke and cognitive impairment, data from 20,243 and 14,175 participants, respectively, were found usable based on the quality of the information from the questionnaires and tests. Approximately one-third of the sample identified as Black and the majority of the remaining two-thirds identified as white.
The results of the study
- According to the authors’ analysis, increasing the intake of ultra-processed foods by just 10% was associated with a significantly greater risk of cognitive impairment and stroke.
- Intake of unprocessed or minimally processed foods was associated with a lower risk of cognitive impairment.
- The effect of ultra-processed foods on stroke risk was greater for individuals who identified as Black compared to individuals who identified as white.
Study participants who reported following a healthy diet (like a Mediterranean, DASH, or MIND diet) and consumed minimal ultra-processed foods appeared to maintain better brain health compared to those who followed similar healthy diets but had more ultra-processed foods.
Why might ultra-processed foods be bad for your brain?
Here are some biologically plausible reasons:
- UPFs are generally composed of processed carbohydrates that are very quickly broken down into simple sugars, equivalent to eating lots of candy. These sugar loads cause spikes of insulin, which can alter normal brain cell function.
- Eating ultra-processed foods is associated with a higher risk of metabolic syndrome and obesity, well-established conditions linked to high blood pressure, abnormal blood lipid levels, and type 2 diabetes.
- There are unhealthy additives in ultra-processed foods to change the texture, color, sweetness, or flavor. These additives disrupt the microbiome in the gut and can lead to gut inflammation that can cause
- the production of microbiome-produced metabolites that can affect brain function (such as short-chain fatty acids and lipopolysaccharides)
- leaky gut, allowing toxins and inflammatory molecules to enter the bloodstream and go to the brain
- altered neurotransmitter function (such as serotonin) that can impact mood and cognition directly
- increased cortisol levels that mimic being under chronic stress, which can directly impact hippocampal and frontal lobe function, affecting memory and executive function performance, respectively
- an increased risk for Alzheimer’s, Parkinson’s, and other neurodegenerative diseases due to inflammatory molecules traveling from the gut to the brain.
- Because ultra-processed foods have poor nutritional value, people will often be hungry shortly after eating them, leading to overeating and its consequences.
The take-home message
Avoid processed foods, which can include chips and other snack foods, industrial breads and pastries, packaged sweets and candy, sugar-sweetened and diet sodas, instant noodles and soups, ready-to-eat meals and frozen dinners, and processed meats such as hot dogs and bologna. Eat unprocessed or minimally processed foods, which — when combined with a healthy Mediterranean menu of foods — include fish, olive oil, avocados, whole fruits and vegetables, nuts and beans, and whole grains.
About the Author
Andrew E. Budson, MD, Contributor; Editorial Advisory Board Member, Harvard Health Publishing
Dr. Andrew E. Budson is chief of cognitive & behavioral neurology at the Veterans Affairs Boston Healthcare System, lecturer in neurology at Harvard Medical School, and chair of the Science of Learning Innovation Group at the … See Full Bio View all posts by Andrew E. Budson, MD

Ever read your medical record? Here’s why you should

Do you ever read the notes written by your doctor or health practitioner during a medical visit? If not, you might want to check them out. Usually, these medical notes are full of helpful insights about your health and reminders of recommendations discussed. And there’s medicalese, of course: hard-to-pronounce illnesses, medications, and technical terms.
But you may be surprised to see incorrect information or unexpected language, tone, or even innuendo. Was your past medical history really that “unremarkable”? Did you actually “deny” drinking alcohol? Did the note describe you as “unreliable”?
Here’s how to decipher unfamiliar lingo, understand some surprising descriptions, and flag any errors you find.
What’s in a medical note?
A standard medical note has several sections. These include
- a description of current symptoms
- past medical problems
- a list of medications taken
- family medical history
- social habits such as smoking, drinking alcohol, or drug use
- details of the physical examination
- test results
- a discussion of the big picture, along with recommendations for further evaluation or treatment.
Notes tend to be more complete for a new patient or annual exam. Follow-up notes may not cover all of these points.
What’s potentially confusing about medical notes?
Most medical notes aren’t written using plain language because they aren’t intended primarily for a nonmedical audience. So it’s common to run across:
- Medical jargon: You had an upset stomach and a fever. Doctors may say “dyspepsia” (upset stomach) and “febrile” (fever).
- Complicated disease names: Ever heard of “multicentric reticulohistiocytosis” or “progressive multifocal leukoencephalopathy?” These are just two of thousands of examples.
- Use of common language in uncommon ways: For example, your medical history might be called “unremarkable” and test results called "within normal limits” rather than “normal.”
- Abbreviations: You might see “VSS” and “RRR,” meaning “vital signs stable” with a pulse that has a “regular rate and rhythm.”
If you’re having trouble deciphering a note or understanding your health issues, tests, and recommendations, check in with your doctor’s office for clarifications. The more you understand about your health and your options for care, the better.
What if a medical note is incorrect?
Minor errors in medical notes are not rare: maybe you had your tonsils removed 30 years ago, not 10 years ago. But there can be more important errors: stating that arthritis in your left knee is severe when it’s actually the right knee that’s severe could lead to having x-rays (or even surgery!) on the wrong side. And not properly recording a family history of cancer or heart disease could mean missing out on timely screening tests or preventive treatments.
In an era of ever-increasing time pressure, use of voice recognition software, electronic record templates, drop-down menus, and ability to copy and paste text, it’s easier than ever for health care providers to make (and perpetuate) errors in the medical record.
If you do see an important error that could affect your health, ask your provider to amend it.
What if the language in a medical note seems offensive?
Numerous studies have highlighted the problem of stigmatizing language in medical notes that can leave people feeling judged or offended. Negative attitudes can affect the quality of our health care and willingness to seek care, and can also widen health disparities. One study linked stigmatizing language to higher rates of medical errors. Of note, this study found higher rates of stigmatizing language and medical error among black patients.
Examples include:
- Depersonalization: A note might describe a patient as “a drug abusing addict” rather than a person struggling with drug addiction.
- Insulting or inappropriate descriptors: Notes might contain subjective descriptions that paint the patient in an unflattering light without providing context. For example, the note might say “the patient is unkempt and is drug-seeking” rather than “the patient is experiencing homelessness and has severe, chronic pain.” If a person’s recall of medical events from the past is hazy, they may be called “unreliable.”
- Dismissiveness: A medical note may suggest a symptom is not real or is exaggerated, rather than taking the complaint seriously.
- An untrusting tone: Language such as “she claims she never drinks” or “he denies alcohol use” may suggest mistrust by the physician.
Why might this happen, anyway?
How does such language make its way into medical notes? (To be clear, these possible explanations are not justifications.)
- Tradition and training: Medical trainees, like other learners, tend to follow the lead of their mentors. So if stigmatizing language is used by an instructor, trainees may do the same.
- Time pressure: With medical documentation (as in most everything else), mistakes are more common if you’re rushing.
- Bias: Like everyone else, doctors have biases, including ones they aren’t aware of. How we are taught to think about people — by family, by society — can spill over into every area of life, including work.
- Frustration: Doctors may feel frustrated by patients who don’t follow their recommendations. That frustration can be reflected in their medical notes. For example, a note may say, “As expected, the patient’s blood sugar is high; he is still not checking his blood sugar or following the diet recommended by his nutritionist.”
If the language in a note is confusing or bothersome, ask about it. The Open Notes movement and federal legislation have given most of us much better access to our medical records. This has worthy goals — greater transparency and better communication with people about their medical care — and unintended consequences.
Is changing language in notes that health practitioners once shared mainly with each other a positive consequence? Mostly. Yet some doctors worry that notes will become less specific, accurate, or useful since they may leave out information that might upset a patient.
The bottom line
I encourage you to read your health providers’ notes about your care. If there is a substantial error or something you find confusing or objectionable, ask about it. By the way, a signed medical note cannot usually be revised. However, your doctor can make clarifications or correct mistakes in an addendum at the end of the note.
As more and more patients read their medical notes, it’s likely that health providers will be more conscientious about the language they use. So, wide access to medical notes may improve not only people’s understanding of their health, but also the quality of notes over time.
It's worth remembering that the medical note is not the most important thing that happens during a visit to your doctor. A great note isn’t the same as great care, and vice versa. Still, your medical notes can be a valuable source of health information that differs from all others, including trusted health sites and social media: they’re written by your doctor and they’re all about you.
About the Author
Robert H. Shmerling, MD, Senior Faculty Editor, Harvard Health Publishing; Editorial Advisory Board Member, Harvard Health Publishing
Dr. Robert H. Shmerling is the former clinical chief of the division of rheumatology at Beth Israel Deaconess Medical Center (BIDMC), and is a current member of the corresponding faculty in medicine at Harvard Medical School. … See Full Bio View all posts by Robert H. Shmerling, MD

Orienteering: Great exercise and better thinking skills?

Picture this: you’re with friends in an unfamiliar forest using only a map and a compass to guide you to an upcoming checkpoint. There are no cell phones or GPS gadgets to help, just good old brainpower fueled by a sense of adventure as you wind through leafy trees and dappled sunlight.
This is not an excursion to a campsite or a treasure hunt. It’s a navigation sport called orienteering — a fun way to get outside, exercise, and maybe even help fight cognitive decline, according to a 2023 study.
What is orienteering?
Orienteering combines map and compass reading with exercise. Competitors (“orienteers”) race against a clock to reach checkpoints in outdoor settings that can range from city parks to remote areas with mountains, lakes, rivers, or snowy fields.
“You can go out in a group or on your own. You get a very detailed map and navigate your way to checkpoints that record your time electronically,” says Clinton Morse, national communications manager with Orienteering USA, the national governing body for the sport in the United States.
Because orienteers are racing the clock, they might run on trails, hike up hills, or scramble around boulders. That’s for foot-orienteering events. There are also orienteering events with courses geared for mountain biking, cross-country skiing, or canoeing.
How might orienteering affect thinking skills?
A small 2023 study published online in PLoS One found a potential link between orienteering and sharp thinking skills.
Researchers asked 158 healthy people, ages 18 to 87, about their health, activities, navigation abilities, and memory. About half of the participants had varying levels of orienteering experience. The other participants were physically active but weren’t orienteers.
Compared with study participants who didn’t engage in orienteering, those who were orienteers reported
- having better navigational processing skills (recognizing where objects were, and where participants were in relation to the objects)
- having better navigational memory skills (recalling routes and landmarks).
The study was observational — that is, not a true experiment — and thus didn’t prove that orienteering boosted people’s thinking skills. But the link might be plausible.
“Aerobic exercise releases chemicals in the brain that foster the growth of new brain cells. And when you use a map and connect it to landmarks, you stimulate growth between brain cells,” says Dr. Andrew Budson, lecturer in neurology at Harvard Medical School and chief of cognitive and behavioral neurology at VA Boston Healthcare System.
Where can you find orienteering opportunities?
There are about 70 orienteering clubs across the United States, and many more around the world (the sport is extremely popular in Europe). To find an orienteering event in your area, use the club finder tool offered by Orienteering USA.
How can you get started with orienteering?
People of all ages and athletic levels can take part, because orienteering courses vary from local parks to wilderness experiences. Costs are about $7 to $10 per person for local events, or $25 to $40 per person for national events, plus any travel and lodging expenses.
To make orienteering easy at first, Morse suggests going with a group and taking things slowly on a short novice course. “You don’t have to race,” he says. “Some people do this recreationally to enjoy the challenge of completing a course at their own pace.”
The trickiest part is learning to read the map. Morse’s advice:
- Turn the map as you change directions. Hold the map so that the direction you’re heading in is at the top of the page. For example, if the compass indicates that you’re heading south, turn the map upside down, so the south part is on top and easier to follow.
- Create a mental image of what the map is telling you. If there’s a fence along a field on the map, build a picture of it in your mind so you can recognize it when you see it, even if you haven’t been there before.
Tips for safe and enjoyable orienteering events:
- Dress appropriately. Wear comfortable clothes including long pants, good walking shoes, and a hat.
- Lather up. You’ll be outside for at least an hour, and you’ll need sunblock and possibly tick and bug spray depending on the terrain. Preventing tick bites that can lead to Lyme disease and other tick-borne illnesses is important in many locations.
- Bring some essentials. Pack water, a snack, sunblock, bug spray, and your phone. (Keep the phone turned off unless you need to call for help.)
- Use good judgment. Know that the shortest route on the map won’t always be the best, since it might take you up a hill or through thick vegetation. It might be better to go around those areas.
Once you learn the basics of orienteering, you can make it more physically challenging (and a better workout) by going faster and trying to beat your previous times, or by signing up for a more advanced course that’s longer and requires more exertion and speed.
And no matter which event you take part in, enjoy the adventure. “You’re not just following a path, you’re solving puzzles while being immersed in nature,” Morse says. “It’s a great way to experience the outdoors.”
About the Author

Heidi Godman, Executive Editor, Harvard Health Letter
Heidi Godman is the executive editor of the Harvard Health Letter. Before coming to the Health Letter, she was an award-winning television news anchor and medical reporter for 25 years. Heidi was named a journalism fellow … See Full Bio View all posts by Heidi Godman
About the Reviewer
Howard E. LeWine, MD, Chief Medical Editor, Harvard Health Publishing
Dr. Howard LeWine is a practicing internist at Brigham and Women’s Hospital in Boston, Chief Medical Editor at Harvard Health Publishing, and editor in chief of Harvard Men’s Health Watch. See Full Bio View all posts by Howard E. LeWine, MD

The cicadas are here: How’s your appetite?

You’ve probably heard the news: Cicadas are coming. Or — wait — they’re already here.
And are they ever! Due to an unusual overlap of the lifecycles of two types (or broods) of cicadas, trillions of cicadas are expected to emerge in the US by the end of June, especially in the Midwest.
If you’d like to see where they’ve already arrived, track them here. And if you’re wondering if this cicada-palooza could help with grocery bills, read on to decide for yourself how appealing and how safe snacking on cicadas is for you. The pros and cons could change your outlook on the impending swarm.
What to know about cicadas
Don’t worry, cicadas are largely harmless to humans. In fact, their appearance is welcome in places where people routinely snack on them as a low-cost source of calories and protein.
Estimates suggest up to two billion people regularly eat insects, especially in South and Central America, Asia, Africa, Australia, and New Zealand. Cicadas, when available, are among the most popular. And if you thought no one in the US eats cicadas, check out this video from a May 2024 baseball game.
Are you tempted to eat cicadas?
For plenty of people, cicadas aren’t the food of choice. Some people can’t get past the idea of eating insects as food. That’s understandable: after all, the culture in which we are raised has a powerful influence on what we consider acceptable in our diets. Something some Americans might find off-putting (such as eating snakes) is common in China and Southeast Asia. Meanwhile, people outside the US find aspects of the typical Western diet unappealing (such as root beer, peanut butter and jelly, and processed cheese).
But some people shouldn’t eat cicadas because it could be dangerous for them.
Why you should — or shouldn’t — eat cicadas
Eating cicadas is common in many parts of the world because they are
- nutritious: cicadas are low in fat and high in protein, including multiple essential amino acids
- inexpensive or free
- tasty (or so I’m told): descriptions of their flavor vary from nutty to citrusy to smoky and slightly crunchy.
In years when cicadas emerge, recipes for dishes containing cicadas emerge as well.
Then again, there are several good reasons to avoid making cicadas a part of your diet, including these:
- You just can’t get past the “ick” factor. Adventurous eaters may be willing to try or even embrace consuming cicadas, while others will be unable to view the idea as anything other than horrifying.
- You find the taste or consistency unappealing.
- You’re “cicada intolerant.” Some people get stomach upset, nausea, or diarrhea if they eat too many cicadas.
- You’re pregnant or breastfeeding, or are a young child. Concerns about even low levels of pesticides or other toxins in cicadas have led to recommendations that these groups not eat them. Doesn’t this suggest the rest of us should also steer clear? Well, thus far, at least, there’s no evidence that toxins in cicadas are causing health problems.
But there is one more very important entry on this list: people with a shellfish allergy should not eat cicadas. Odd, right?
The shellfish-cicada connection
Cicadas are biologically related to lobsters, shrimp, crabs, and other shellfish. So if you’re allergic to shellfish, you might also be allergic to cicadas. A particular protein called tropomyosin is responsible for the allergy. It’s found in shellfish as well as in many insects, including cicadas.
The allergic reaction occurs after eating the cicada. Just being around them or handling them won’t trigger a reaction.
Among people with a shellfish allergy, developing a reaction after eating cicadas could be a bigger problem than it seems: up to 10% of people have shellfish allergies and, as noted, insect consumption is common worldwide.
Is it okay for your dog or cat to eat cicadas?
Walking your dog after the emergence of cicadas can be a new and exciting experience for you and your pet! Dogs may chase after cicadas and eat them. Cats might, too, if given the chance. That can be a problem if your pet eats too many, as some will experience stomach upset or other digestive problems.
While the insects are considered harmless to dogs, the American Kennel Club says it’s best to steer them away from cicadas once they’ve eaten a few.
Which other insects trigger allergies?
While insect-related allergic reactions (think bee stings) and infections (like Lyme disease) are well known, the insect-food-allergy connection is a more recent discovery.
One recently recognized condition is the alpha-gal syndrome, in which a person bitten by certain ticks develops an allergy to meat. The name comes from a sugar called galactose-α-1,3-galactose (or alpha-gal) found in many types of meat including beef, lamb, pork, and rabbit. According to the CDC, up to 450,000 people in the US may have developed this condition since 2010.
There aren’t many rigorous studies of the overlap of insects and food allergies, so there are probably others awaiting discovery.
The bottom line
When it comes to eating cicadas, I’ll pass. It’s not because of the risks. I’ve never had a problem with shellfish, and for most people the health risks of eating cicadas seem quite small. It’s just unappealing to me, and I’m not a particularly adventurous eater.
But let’s go easy on those who do enjoy snacking on cicadas. Insects offer a good source of calories and protein. Just because eating them seems unusual in the US doesn’t make it wrong.
So, if you like to eat cicadas and have no shellfish allergy or other reason to avoid them, go for it! This may be a very good summer for you.
About the Author
Robert H. Shmerling, MD, Senior Faculty Editor, Harvard Health Publishing; Editorial Advisory Board Member, Harvard Health Publishing
Dr. Robert H. Shmerling is the former clinical chief of the division of rheumatology at Beth Israel Deaconess Medical Center (BIDMC), and is a current member of the corresponding faculty in medicine at Harvard Medical School. … See Full Bio View all posts by Robert H. Shmerling, MD
What is cognitive behavioral therapy?
Cognitive behavioral therapy (CBT) teaches people to challenge negative thought patterns and turn less often to unhelpful behaviors. These strategies can improve your mood and the way you respond to challenging situations: a flat tire, looming deadlines, family life ups and downs.
Yet there’s much more depth and nuance to this well-researched form of psychotherapy. It has proven effective for treating anxiety, depression, and other mental health conditions. Tailored versions of CBT can also help people cope with insomnia, chronic pain, and other nonpsychiatric conditions. And it can help in managing difficult life experiences, such as divorce or relationship problems.
What are the key components of CBT?
One important aspect of CBT relates to perspective, says psychologist Jennifer Burbridge, assistant director of the Cognitive Behavioral Therapy Program at Harvard-affiliated Massachusetts General Hospital.
“Therapists who practice CBT don’t see the problems or symptoms people describe as having one single cause, but rather as a combination of underlying causes,” she says. These include
- biological or genetic factors
- psychological issues (your thoughts, physical sensations, and behaviors)
- social factors (your environment and relationships).
Each of these factors contributes to — and helps maintain — the troublesome issues that might prompt you to seek therapy, she explains.
How does CBT describe our emotions?
Our emotions have three components: thoughts, physical sensations, and behaviors.
“Thoughts are what we say to ourselves, or 'self-talk,'” says Burbridge. Physical sensations are what we observe in our bodies when we experience an emotional situation: for example, when your heart rate rises in stressful circumstances. Behaviors are simply the things you do — or do not do. For instance, anxiety might prevent you from attending a social event.
All three components are interrelated and influence one another. That’s why CBT helps people to develop skills in each of them. “Think of it as a wellness class for your emotional health,” says Burbridge.
How long does CBT last?
CBT is a goal-oriented, short-term therapy. Typically it involves weekly, 50-minute sessions over 12 to 16 weeks. Intensive CBT may condense this schedule into sessions every weekday over one to three weeks.
Is CBT collaborative?
“When I first meet with someone, I’ll listen to what’s going on with them and start thinking about different strategies they might try,” Burbridge says. But CBT is a collaborative process that involves homework on the patient’s part.
What might that mean for you? Often, a first assignment involves self-monitoring, noting whether there are certain things, events, or times of day that trigger your symptoms. Future sessions focus on fine-tuning approaches to elicit helpful, adaptive self-talk, and problem-solving any obstacles that might prevent progress.
Certain thinking patterns are often associated with anxiety or depression, says Burbridge. Therapists help people recognize these patterns and then work with patients to find broader, more flexible ways to cope with difficult situations.
“We’re cognitive creatures with big frontal lobes that help us analyze situations and solve problems. That’s useful in some situations. But at other times, when you’re trying to manage your emotions, it may be better to pause and acknowledge and accept your discomfort,” says Burbridge.
Which CBT tools and strategies can help?
That particular skill — paying attention in the present moment without judgement, or mindfulness — is a common CBT tool. Another strategy that’s helpful for anxiety, known as exposure or desensitization, involves facing your fears directly.
“People avoid things that make them nervous or scared, which reinforces the fear,” says Burbridge. With small steps, you gradually expose yourself to the scary situation. Each step provides learning opportunities — for example, maybe you realize that the situation wasn’t as scary as you though it would be.
By trying new things instead of avoiding them, you begin to change your thought patterns. These more adaptive thinking patterns then make it more likely you will try new or challenging experiences in the future, thereby increasing your self-confidence.
How does CBT work?
Brain imaging research suggests conditions like depression or anxiety change patterns of activity in certain parts of the brain. One way CBT may help address this is by modifying nerve pathways involved in fear responses, or by establishing new connections between key parts of the brain.
A 2022 review focused on 13 brain imaging studies of people treated with CBT. The analysis suggested CBT may alter activity in the prefrontal cortex (often called the “personality center”) and the precuneus (which is involved in memory, integrating perceptions of the environment, mental imagery, and pain response).
Who might benefit from CBT?
CBT is appropriate for people of all different ages. This can range from children as young as 3 years — in tandem with parents or caregivers — to octogenarians. In addition to treating anxiety and depression, CBT is also effective for
- eating disorders
- substance abuse
- personality disorders
- attention deficit hyperactivity disorder (ADHD)
- obsessive compulsive disorder (OCD).
Additional evidence shows CBT may help people with different health issues, including irritable bowel syndrome, chronic fatigue syndrome, fibromyalgia, insomnia, migraines, and other chronic pain conditions. The therapy may also benefit people with cancer, epilepsy, HIV, diabetes, and heart disease.
“Many medical conditions can limit your activities. CBT can help you adjust to your diagnosis, cope with the new challenges, and still live a meaningful life, despite the limitations,” says Burbridge.
About the Author

Julie Corliss, Executive Editor, Harvard Heart Letter
Julie Corliss is the executive editor of the Harvard Heart Letter. Before working at Harvard, she was a medical writer and editor at HealthNews, a consumer newsletter affiliated with The New England Journal of Medicine. She … See Full Bio View all posts by Julie Corliss
About the Reviewer
Howard E. LeWine, MD, Chief Medical Editor, Harvard Health Publishing
Dr. Howard LeWine is a practicing internist at Brigham and Women’s Hospital in Boston, Chief Medical Editor at Harvard Health Publishing, and editor in chief of Harvard Men’s Health Watch. See Full Bio View all posts by Howard E. LeWine, MD

Power your paddle sports with three great exercises

On the Gulf Coast of Florida where I live, the telltale sign of summer is not an influx of beachcombers, afternoon storms that arrive exactly at 2 p.m., or the first hurricane warning, but the appearance of hundreds of paddleboarders dotting the inlet waters.
From afar, paddleboarding looks almost spiritual — people standing on nearly invisible boards and gliding across the surface as if walking on water.
But this popular water sport offers a serious workout, just as kayaking and canoeing do. While floating along and casually dipping a paddle in the water may look effortless, much goes on beneath the surface, so to speak.
As warm weather beckons and paddle season arrives, it pays to get key muscles in shape before heading out on the water.
Tuning up muscles: Focus on core, back, arms, and shoulders
“Paddling a kayak, canoe, or paddleboard relies on muscles that we likely haven’t used much during winter,” says Kathleen Salas, a physical therapist with Spaulding Adaptive Sports Centers at Harvard-affiliated Spaulding Rehabilitation Network. “Even if you regularly weight train, the continuous and repetitive motions involved in paddling require endurance and control of specific muscles that need to be properly stretched and strengthened.”
While paddling can be a whole-body effort (even your legs contribute), three areas do the most work and thus need the most conditioning: the core, back, and arms and shoulders.
- Core. Your core comprises several muscles, but the main ones for paddling include the rectus abdominis (that famed “six-pack”) and the obliques, located on the side and front of your abdomen. The core acts as the epicenter around which every movement revolves — from twisting to bending to stabilizing your trunk to generate power.
- Back: Paddling engages most of the back muscles, but the ones that carry the most load are the latissimus dorsi muscles, also known as the lats, and the erector spinae. The lats are the large V-shaped muscles that connect your arms to your vertebral column. They help protect and stabilize your spine while providing shoulder and back strength. The erector spinae, a group of muscles that runs the length of the spine on the left and right, helps with rotation.
- Arms and shoulders: Every paddle stroke engages the muscles in your arms (biceps) and the top of your shoulder (deltoids).
Many exercises specifically target these muscles, but here are three that can work multiple paddling muscles in one move. Add them to your workouts to help you get ready for paddling season. If you haven’t done these exercises before, try the first two without weights until you can do the movement smoothly and with good form.
Three great exercises to prep for paddling
Wood chop


Muscles worked: Deltoids, obliques, rectus abdominis, erector spinae
Reps: 8–12 on each side
Sets: 1–3
Rest: 30–90 seconds between sets
Starting position: Stand with your feet about shoulder-width apart and hold a dumbbell with both hands. Hinge forward at your hips and bend your knees to sit back into a slight squat. Rotate your torso to the right and extend your arms to hold the dumbbell on the outside of your right knee.
Movement: Straighten your legs to stand up as you rotate your torso to the left and raise the weight diagonally across your body and up to the left, above your shoulder, while keeping your arms extended. In a chopping motion, slowly bring the dumbbell down and across your body toward the outside of your right knee. This is one rep. Finish all reps, then repeat on the other side. This completes one set.
Tips and techniques:
- Keep your spine neutral and your shoulders down and back
- Reach only as far as is comfortable.
- Keep your knees no farther forward than your toes when you squat.
Make it easier: Do the exercise without a dumbbell.
Make it harder: Use a heavier dumbbell.
Bent-over row


Muscles worked: Latissimus dorsi, deltoids, biceps
Reps: 8–12
Sets: 1–3
Rest: 30–90 seconds between sets
Starting position: Stand with a weight in your left hand and a bench or sturdy chair on your right side. Place your right hand and knee on the bench or chair seat. Let your left arm hang directly under your left shoulder, fully extended toward the floor. Your spine should be neutral, and your shoulders and hips squared.
Movement: Squeeze your shoulder blades together, then bend your elbow to slowly lift the weight toward your ribs. Return to the starting position. Finish all reps, then repeat with the opposite arm. This completes one set.
Tips and techniques:
- Keep your shoulders squared throughout.
- Keep your elbow close to your side as you lift the weight.
- Keep your head in line with your spine.
Make it easier: Use a lighter weight.
Make it harder: Use a heavier weight.
Superman


Muscles worked: Deltoids, latissimus dorsi, erector spinae
Reps: 8–12
Sets: 1–3
Rest: 30–90 seconds between sets
Starting position: Lie face down on the floor with your arms extended, palms down, and legs extended.
Movement: Simultaneously lift your arms, head, chest, and legs off the floor as high as is comfortable. Hold. Return to the starting position.
Tips and techniques:
- Tighten your buttocks before lifting.
- Don’t look up.
- Keep your shoulders down, away from your ears.
Make it easier: Lift your right arm and left leg while keeping the opposite arm and leg on the floor. Switch sides with each rep.
Make it harder: Hold in the “up” position for three to five seconds before lowering.
About the Author

Matthew Solan, Executive Editor, Harvard Men's Health Watch
Matthew Solan is the executive editor of Harvard Men’s Health Watch. He previously served as executive editor for UCLA Health’s Healthy Years and as a contributor to Duke Medicine’s Health News and Weill Cornell Medical College’s … See Full Bio View all posts by Matthew Solan
About the Reviewer
Howard E. LeWine, MD, Chief Medical Editor, Harvard Health Publishing
Dr. Howard LeWine is a practicing internist at Brigham and Women’s Hospital in Boston, Chief Medical Editor at Harvard Health Publishing, and editor in chief of Harvard Men’s Health Watch. See Full Bio View all posts by Howard E. LeWine, MD

How health care leaders can prioritize health equity for the LGBTQIA2+ community

Editor's note: Health inequities have long been an issue for people in the LGBTQ+ community. We're pleased to share a post from our colleagues in Corporate Learning at Harvard Medical School focusing on solutions that health care leaders can champion.
Health care business professionals can improve patient outcomes and reduce health inequities by championing the health care needs of the lesbian, gay, bisexual, transgender, queer and/or questioning, intersex, asexual, and two-spirit (LGBTQIA2+) community. These issues are an important priority for health care professionals year-round, not just during Pride Month.
Research shows that the LGBTQIA2+ community faces disproportionate adverse health conditions due to health inequities. It’s important for those working in the health care industry to be aware of the challenges the LGBTQIA2+ community faces to help make systemic changes and improve health outcomes.
The LGBTQIA2+ community — which is less likely to trust the health care system — is a rising part of the population. The 2022 national Gallup survey shows that at least 20% of Gen Z identifies as LGBTQIA2+. This includes our coworkers, customers, and clients, says Dr. Alex Keuroghlian, a psychiatrist at Massachusetts General Hospital and faculty advisor for LGBT and Allies at Harvard Medical School (LAHMS).
“LGBTQIA2+ people experience pervasive stigma and discrimination, as well as numerous adverse social determinants of health, all of which negatively impact health outcomes,” says Dr. Keuroghlian. “Health care professionals, organizations, and governmental agencies need to intentionally provide clinical care and design health systems and policies, in a manner that is culturally responsive and improves health outcomes for LGBTQIA2+ people.”
Due to the politicized nature of these issues, health care providers around the world, including in several U.S. states, face limitations and backlash when providing gender-affirming care. In some places, Dr. Keuroghlian says, “legal restrictions on access to gender-affirming care create challenges for clinicians to deliver this care and for transgender and gender diverse people to safely receive it.”
Everyone in health care — including health care business professionals — can work to improve health outcomes and decrease inequities. “It is critical for all businesses to offer welcoming, inclusive, and affirming work environments and service delivery for LGBTQIA2+ people,” Dr. Keuroghlian says.
Supporting LGBTQIA2+ health begins in the workplace
With thoughtful action, health care business professionals can contribute to greater health equity for these underserved individuals. Some ways to do so include:
1. Take an active interest in better understanding the needs and perspectives of the LGBTQIA2+ community.
Conducting research, including surveys and consumer focus groups, is a good way to help better understand specific health needs and priorities. “This community has historically been excluded from studies and research that would be very helpful in understanding their needs and their challenges,” says Dr. Enrique Caballero, an endocrinologist at Brigham and Women’s Hospital and the faculty director of International Innovation Programs in the HMS Office for External Education. “We need to get to know the population better.”
2. Prioritize inclusive language.
Whether you are involved directly in care delivery or other aspects of health care, pay attention to the words you use — for both customers and employees. Gendered language in job postings, informational or marketing materials, and even casual conversation can be off-putting. That means lost opportunities for organizations and LGBTQIA2+ individuals. Slight shifts in language and conscious efforts like adding pronouns to your email signature speak volumes.
3. Train staff to be community allies.
Gaining awareness of our unconscious biases and making shifts in our everyday language doesn’t happen overnight. Health care industry businesses can help their staff be better allies to the LGBTQIA2+ community by providing access to workshops delivered by community members.
“No one becomes fully competent after one conversation, lecture, or video,” Dr. Caballero says. “It’s a lifelong process in which we all learn how to be more respectful, inclusive, and to embrace diversity.”
4. Support companies and community organizations that focus on LGBTQIA2+ health.
Show, don’t tell. Making financial contributions to organizations already on the ground and working with this population demonstrates that you aren’t just concerned about the bottom line. You are truly dedicated to helping the LGBTQ+ population access good health care.
5. Hire LGBTQIA2+ staff.
The best way to ensure your company is prioritizing health equity is by having a diverse group at the decision-making table. It is crucial to have employees that represent the diversity of your customer base — not only diversity in gender expression and sexuality, but also diversity in race, ethnicity, age, ability, and beyond.
“Part of our obligation is to really open the doors for everybody,” Dr. Caballero says. “Talent is not exclusive to a particular group, and I think that is important to embrace as an organization.”
6. Include LGBTQIA2+ representation in all communications.
Diverse representation is key. Make a pointed effort to include same-sex couples, non-traditional family units, and transgender and non-binary individuals in all kinds of communications, participating in everyday activities.
7. Acknowledge any missteps.
On an institutional level, company acknowledgments can go a long way in rebuilding trust with the LGBTQIA2+ community. Within the organization, it’s valuable to encourage ongoing communication about company culture.
“All organizations should have a system in place for people to provide feedback on how things are going and to report anything that they want to call the leadership team's attention to,” Dr. Caballero says. “Having a system that truly listens to members of the organization — and being sure that follow-up action is taken — is very important.”
8. Make action consistent beyond Pride Month.
Embracing the LGBTQIA2+ community consistently and with commitment all year long “is truly an opportunity for everyone,” Dr. Caballero says. “This is not good just for the members of the community, but for everybody that works in a place that embraces diversity, equity, and inclusion.”
Industry professionals turn to HMS for custom corporate learning programs, including on topics like LGBTQIA2+ health, that leave a lasting impact on participants. To provide these programs, HMS leverages faculty expertise from throughout the School and the entire Harvard University community to share with health care teams. To learn about HMS Corporate Learning custom programs, read about the approach or hear from clients themselves.
About the Author
Corporate Learning Staff
Harvard Medical School’s Corporate Learning solutions provide emerging and established companies with the knowledge they need to address the industry's toughest business challenges. Their extensive portfolio of learning solutions helps teams achieve their potential by advancing … See Full Bio View all posts by Corporate Learning Staff

Prostate cancer: Brachytherapy linked to long-term risk of secondary malignancies

When cancer patients are treated with radiation, it’s possible that the therapy itself may cause new tumors to form in the body later. Radiation kills cancer cells by damaging their DNA, but if the treatments cause genetic damage to normal cells near the radiation target, there’s a small risk that these secondary malignancies may arise over time.
Just over 10 years ago, Canadian researchers set out to assess the risk of secondary malignancy among men with prostate cancer who were treated with a type of radiation called brachytherapy. Unlike radiation delivered from sources outside the body, brachytherapy is accomplished by implanting dozens of radioactive pellets, or “seeds,” directly into the tumor site. Those seeds, which are never removed, emit radiation at a dose that declines toward zero over the course of a year.
Brachytherapy has the advantage of convenience. Instead of traveling for repeat sessions of radiation, men need only one treatment, usually given in an outpatient setting. But brachytherapy is also falling out of favor, in part because newer types of external beam radiation deliver high-precision doses with fewer side effects.
Study methodology and results
The Canadian study compared rates of secondary malignancies in the pelvis among men treated either with brachytherapy or with surgery to remove the prostate. All the treatments took place in British Columbia between 1998 and 2000. The brachytherapy group included 2,418 men with an average age of 66, while the surgically-treated group contained 4,015 men whose average age was 62. Within that group, 2,643 men had been treated with surgery alone, and 1,372 men with surgery plus external beam radiation given later.
After median follow-ups of between 5.8 years (brachytherapy) and 6.4 years (surgery), the study team reported in 2014 that there was no difference in rates of secondary malignancies between the groups, or with cancer incidence in the general population.
But that’s no longer the case: In April 2024, the researchers published updated findings. This time, rates of new cancers in the pelvis — including the bladder and rectum — were higher in the brachytherapy group. Specifically, 6.4% of brachytherapy-treated men had secondary malignancies at 15 years of follow-up, increasing to 9.8% after 20 years. By contrast, 3.2% and 4.2% of surgically-treated men developed secondary pelvic malignancies over the same durations. There was no difference in deaths from secondary malignancies between the groups.
The strength of the association with bladder cancer in particular is “similar to that seen with smoking,” wrote the author of an accompanying editorial. Results from the study “should be considered when treating men with localized prostate cancer who have a long life expectancy,” the authors concluded.
Commentary from experts
“I do believe that this study reveals a dark truth about radiation for prostate cancer that has been long suspected,” says Dr. Anthony Zietman, a professor of radiation oncology at Harvard Medical School and Massachusetts General Hospital, and a member of the advisory and editorial board for the Harvard Medical School Guide to Prostate Diseases. “As the decades pass after radiation therapy of any kind — brachytherapy or external beam — the risk for radiation-induced malignancies rises.
“These malignancies are usually in adjacent organs like the bladder and rectum, or within the prostate itself. They may be very curable, and thus the survival rates are the same for radiation or surgically treated patients, but there is little doubt that, for these patients, they represent a ‘sting in the tail’ long after the radiation has been given and forgotten. This data certainly gives us pause when offering radiation to very young men with several decades of life expectancy ahead of them, and it also reminds us of the value of follow-up visits.”
“The fact that second cancers arise in the area where radiation was given is not surprising, but the magnitude of the long-term increases is concerning,” added Dr. Marc Garnick, the Gorman Brothers Professor of Medicine at Harvard Medical School and Beth Israel Deaconess Medical Center, and editor in chief of the Harvard Medical School Guide to Prostate Diseases. “There are other common and troublesome urinary side effects of brachytherapy — independent of second cancers — that patients should fully consider before selecting it as a treatment option. This is especially true given the availability of other convenient and similarly effective prostate cancer therapies.”
About the Author

Charlie Schmidt, Editor, Harvard Medical School Annual Report on Prostate Diseases
Charlie Schmidt is an award-winning freelance science writer based in Portland, Maine. In addition to writing for Harvard Health Publishing, Charlie has written for Science magazine, the Journal of the National Cancer Institute, Environmental Health Perspectives, … See Full Bio View all posts by Charlie Schmidt
About the Reviewer
Marc B. Garnick, MD, Editor in Chief, Harvard Medical School Annual Report on Prostate Diseases; Editorial Advisory Board Member, Harvard Health Publishing
Dr. Marc B. Garnick is an internationally renowned expert in medical oncology and urologic cancer. A clinical professor of medicine at Harvard Medical School, he also maintains an active clinical practice at Beth Israel Deaconess Medical … See Full Bio View all posts by Marc B. Garnick, MD
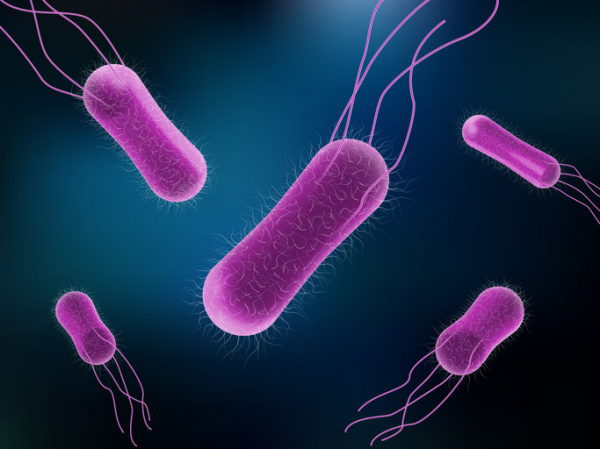
Salmonella is sneaky: Watch out
Pop quiz: what is Salmonella? If you’ve ever had a run-in with this bacteria, you know it can cause a food-borne illness called salmonellosis, a form of food poisoning. But you may not know that Salmonella bacteria sicken an estimated 1.35 million people and hospitalize 26,500 every year in the United States. What’s more, it kills more total people than any other type of food poisoning.
And Salmonella bacteria can be sneaky — not only by triggering unusual complications, but infecting people in startling ways, says Dr. Elizabeth Hohmann, an infectious disease specialist at Massachusetts General Hospital. One patient she treated showed up with an abdominal aortic aneurysm — a dangerous bulge in the lower section of the body’s largest artery — that looked infected. Testing revealed a culprit some would find surprising: Salmonella.
“It’s just an interesting organism and it can be kind of scary,” she says.
How do people get infected by Salmonella?
Many of the foods Salmonella bacteria lurk in are raw or undercooked. Breaded raw chicken products like nuggets and chicken Kiev are one way it may reach your table. But a variety of foods have been implicated — including organic basil, cantaloupes, ground beef, nut butters, raw cookie dough, eggs, raw or unpasteurized milk, and flour.
Even small pets such as turtles and frogs, along with dog food, have contributed to Salmonella outbreaks in recent years.
You can also become infected by handling contaminated food and spreading the bacteria from your hands to your mouth. Additionally, you can spread it to others on your hands or even on your clothes without becoming sick yourself.
“It’s a bug that’s carried in stool and animal feces and is also present in the environment,” Dr. Hohmann says. “So it can set up shop in lots of different inanimate objects, soils, and machinery, especially in moist environments.”
What symptoms can Salmonella cause?
Most of the time, Salmonella infection leads to gastroenteritis, usually causing just an upset stomach, abdominal cramps, and diarrhea. These symptoms can start as soon as six hours after ingesting the bacteria. Typically, symptoms resolve on their own within two to three days.
Some people have such mild symptoms they’re barely noticeable. “The classic case might be a college student who eats a burrito from a sketchy place, gets sick for a couple of days, gets better, and doesn’t think anything of it,” says Dr. Hohmann.
Sometimes symptoms are more serious, such as severe abdominal cramping and bloody diarrhea, or unexplained high fever and marked fatigue. These symptoms require a call to your doctor.
How is salmonellosis treated?
Most people will get better on their own without any medicines. Replacing lost fluids by sipping water or electrolyte drinks to avoid dehydration will help.
Call a doctor if you have
- diarrhea and a fever higher than 102° F
- diarrhea that doesn’t improve after three days
- bloody stools
- vomiting so severe it prevents you from keeping liquids down.
Treating the infection with medicine comes with an annoying paradox, Dr. Hohmann says. If doctors decide to prescribe antibiotics, the person taking the medicine may shed the organism for longer than if they were never treated. “Then that person may have the opportunity — either through poor personal hygiene, sex, or working as a food worker — to spread it to others,” she explains. “It’s challenging.”
What complications can Salmonella lead to?
Some people get sicker with salmonellosis than others, with seemingly no rhyme or reason. But certain folks are especially vulnerable to serious infection, including:
- adults 65 and older
- pregnant women
- children under 5
- people whose immune systems are weakened by diseases (such as cancer) or treatments (such as immunosuppressing drugs).
A small percentage of those infected can have Salmonella in their blood, which can spread the infection to other parts of the body such as the urinary tract, bones, joints, or central nervous system (brain and spinal fluid).
And, like Dr. Hohmann’s patient with the abdominal aortic aneurysm, on rare occasions Salmonella can lead to unusual blood vessel complications in people who already have atherosclerosis, blockage of the arteries caused by plaque buildup.
“It’s not that common,” she says. “Many physicians are aware of it, so they take special care if Salmonella is found in a person with vascular disease.”
What steps can you take to avoid Salmonella?
While new USDA rules that take effect in 2025 may help fuel recalls of certain foods, we all can take steps to avoid the food poisoning, illness, and hospitalizations that Salmonella exposure can cause.
Dr. Hohmann and the CDC suggest these strategies:
- Using hot water and soap, wash cutting boards or plates on which you cut into raw foods — including vegetables and fruit — before using those surfaces for other purposes. If possible, use separate cutting boards for produce, meat, and fish.
- Refrigerate or freeze foods that are perishable, prepared, or left over within two hours to thwart salmonella growth.
- Always wash hands well with soap and water before preparing food and after contact with animals, using the toilet, or changing diapers.
- If you have a sick pet, take extra care handling its feces and wash your hands thoroughly afterward.
Take additional steps to help more vulnerable people stay healthy:
- Don’t let young children touch high-risk animals, such as turtles, frogs, chickens, or ducks. “And if you’re taking young children to a petting zoo, they should not be petting animals unless you can disinfect their hands immediately afterward,” she says.
- Older adults and those with compromised immune systems should take extra care to wash and cook foods thoroughly.
- People who have had a transplant (such as a kidney transplant) should not keep reptiles or amphibians as pets.
“You hate to make people paranoid, so that we’re washing our lettuce leaves with soap, but it’s worth thinking about these things, particularly if you have people in your household who are susceptible — which is an increasing number of people,” Dr. Hohmann says.
About the Author

Maureen Salamon, Executive Editor, Harvard Women's Health Watch
Maureen Salamon is executive editor of Harvard Women’s Health Watch. She began her career as a newspaper reporter and later covered health and medicine for a wide variety of websites, magazines, and hospitals. Her work has … See Full Bio View all posts by Maureen Salamon
About the Reviewer
Howard E. LeWine, MD, Chief Medical Editor, Harvard Health Publishing
Dr. Howard LeWine is a practicing internist at Brigham and Women’s Hospital in Boston, Chief Medical Editor at Harvard Health Publishing, and editor in chief of Harvard Men’s Health Watch. See Full Bio View all posts by Howard E. LeWine, MD